Study of Bone Mineral Density in Transfusion Dependent Thalassemia, its correlation with Biochemical and Hematological parameters: A Cross-Sectional Study
Abstract
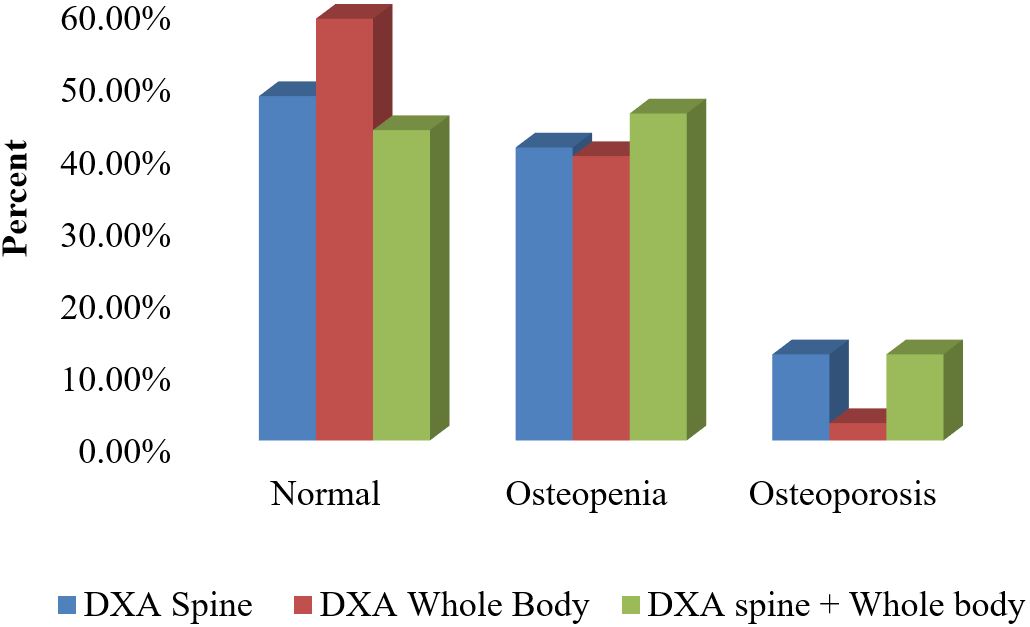
Background: In thalassemic patients, bone disease is an important cause of morbidity. Patients with transfusion-dependent thalassemia (TDT) are susceptible to osteopenia and osteoporosis, the mechanism being multi-factorial. The present study was undertaken to study the prevalence of osteopenia and osteoporosis in TDT patients and describe its correlation with biochemical, hematological profile. Method: A total of 84 patients with TDT on regular PRC transfusion and iron chelation therapy aged between 5-18years were enrolled in the study. Bone mineral densities (BMD) was measured by DXA scan (DXA spine/whole body) and categorized into normal, osteopenia and osteoporosis based on WHO grading system. Results: Out of 84 subjects, 57.1% had low BMD with 38(45.2%) having osteopenia and 10(11.9%) of them having osteoporosis. The prevalence of osteoporosis was found to be more by DXA Spine than DXA whole body which was found to be statistically significant (P=0.043). A high prevalence of hypoparathyroidism, hypocalcemia, hypovitaminosis D and increased serum phosphorous levels were noted among TDT patients with low BMD. Iron overload in Myocardium by T2*MRI also showed statistically significant association with low BMD as determined by DXA Spine. Conclusion: Low bone mass is one of the most prevalent complications among TDT patients. Osteoporosis is a progressive disease with multifactorial etiology. Iron overload status by T2* Cardiac MRI may be used as an early indicator for predicting Osteoporosis along with T-scores from DXA spine for early diagnosis and interventions. Further longitudinal prospective studies are needed to better understand the etiopathogenesis of bone disease in these patients.
Downloads
References
2. Vogiatzi MG, Macklin EA, Fung EB, Cheung AM, Vichinsky Eet al. Bone disease in Thalassemia: A frequent .and still unresolved problem. J Bone Miner Res.2009;24(3):543-557.
3. Maria Domenica Cappellini, Alan Cohen, John Porter, Ali Taher VV. Guidelines for the Management of Transfusion Dependent Thalassaemia (TDT) 3rd Edition. Thalassaemia International Federation. 2014.
4. Leib E. Nomenclature and Decimal Places in Bone Densitometry. In: Journal of Clinical Densitometry. 2004.7(1) 45-49.
5. Bejaoui M, Guirat N. Beta thalassemia major in a developing country: Epidemiological, clinical and evolutionary aspects. Mediterr J Hematol Infect Dis. 2013; 5(1).
6. Merchant R, Udani A, Puri V. Evaluation of Osteopathy in Thalassemia by Bone Mineral Densitometry and Evaluation of Osteopathy in Thalassemia by Bone Mineral Densitometry and Biochemical Indices. 2010;(June 2014). 74(3) 1-320.
7. Borgna-Pignatti C, Stefano P De, Zonta L, Vullo C, Sanctis V De, Melevendi C, et al. Growth and sexual maturation in thalassemia major. J Pediatr. 1985; 106(1) 150-155.
8. Asadi-Pooya AA, Karamifar H. Body mass index in children with betathalassemia major. Turkish J Haematol. 2004; 21(4) 177-18.
9. Pemde H, Chandra J, Singh V, Gupta D, Sharma R, Dutta AK. Physical growth in children with transfusion-dependent thalassemia. Pediatr Heal Med Ther. 2011;13.
10. Jain DC, Bhargav DAK, Pawan DK. Correlation of liver enzymes and haematological profile in thalassemia major patients. Int J Med Res Rev. 2015; 3(10) 1224-1227.
11. Jensen CE, Tuck SM, Agnew JE, Koneru S, Morris RW, Yardumian A, et al. High prevalence of low bone mass in thalassaemia major. Br J Haematol. 1998; 103(4) 911-915.
12. Abdelrazik N, Ghanem H. Failure of puberty in Egyptian beta thalassemic patients: Experience in north east region - Dakahlia province. Hematology. 2007; 12(5) 449-456.
13. Moayeri H, Oloomi Z. Prevalence of growth and puberty failure with respect to growth hormone and gonadotropins secretion in beta-thalassemia major. Arch Iran Med. 2006;9(4) 329-334.
14. De Sanctis V, Elsedfy H, Soliman A, Elhakim I, Soliman N, Elalaily R, et al. Endocrine profile of β-thalassemia major patients followed from childhood to advanced adulthood in a tertiary care center. Indian J Endocrinol Metab. 2016; 20(4) 451-459.
15. Amit J, Radha G, Mamta M, Yashwant G et al. To Study Renal Dysfunction In Children And Adolescents With Thalassemia Major. PediatrHematol Oncol J. 2019; 4(2) S59.
16. El-nashar M, Kamel A, El-beblawy NMS, El-gohary E, Mokhtar I, Rashad M, et al. Parathyroid hormone in pediatric patients with b -thalassemia major and its relation to bone mineral density ; a case control study. Egypt J Med Hum Genet. 2017;18(1):75–8.
17. Saboor M. Levels of Calcium, Corrected Calcium, Alkaline Phosphatase and Inorganic Phosphorus in Patients’ Serum with β-Thalassemia Major on Subcutaneous Deferoxamine. J Hematol Thromboembolic Dis. 2014; 02(02)
18. Rossi F, Perrotta S, Bellini G, Luongo L, Tortora C, Siniscalco D, et al. Iron overload causes osteoporosis in thalassemia major patients through interaction with transient receptor potential vanilloid type 1 channels. Haematologica. 2014; 99(12) 1876-1884.
19. Fernandes JL. MRI for Iron Overload in Thalassemia. Hematology/Oncology Clinics of North America. 2018. 32;277–295.
20. Lotz JC, Cheal EJ, Hayes WC. Fracture prediction for the proximal femur using finite element models: Part I-linear analysis. J Biomech Eng. 1991; 113(4) 353- 360.
21. Pollak RD, Rachmilewitz E, Blumenfeld A, Idelson M, Goldfarb AW. Bone mineral metabolism in adults with beta-thalassaemia major and intermedia. Br J Haematol [Internet]. 2000;111(3):902–7.
22. Karimi M, Ghiam AF, Hashemi A, Alinejad S, Soweid M, Kashef S. Bone Mineral Density in Beta-Thalassemia Major and Intermedia. 2007;44:29–32.
23. Vogiatzi MG, Autio KA, Mait JE, Schneider R, Lesser M, Giardina PJ. Low bone mineral density in adolescents with β-thalassemia. In: Annals of the New York Academy of Sciences. 2005. 1054;462-466.
24. Goh KG, Ahlam NK, Miza HZ, Seman MR. Correlation of iron overload markers, MRI T2-star liver/heart and bone mineral densitometry in transfusiondependent thalassemia patients. Osteoporos Int. 2019; 30; S77-S78.
25. Ebrahimpour L, Akhlaghpoor S, Azarkayvan A, Salehi M, Morteza A, Alinaghi R. Correlation between bone mineral densitometry and liver/heart iron overload evaluated by quantitative T2* MRI. Hematology. 2012; 17(5) 297-301.
26. Massoumeh MH Zadeh et al Osteoporosis and Associated Factors among Thalassemia Patients Referred to Bone Mineral Density Screening -Dubai Hospital, 2014-2017 Clin Case Rep Rev, Volume 3(10): 1-4.
27. Melton LJ, Looker AC, Shepherd JA, O’Connor MK, Achenbach SJ, Riggs BL, et al. Osteoporosis assessment by whole body region vs. site-specific DXA. Osteoporos Int. 2005; 16(12) 1558-1564.
28. Mohseni F, Mohajeri-Tehrani MR, Larijani B, Hamidi Z. Relation between BMD and biochemical, transfusion and endocrinological parameters in pediatric thalassemic patients. Arch Osteoporos. 2014; 9(1).
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


