Pattern of Congenital Anomalies among Pediatric Surgical Patients in Bangladesh
Abstract
Background:Congenital anomalies are structural or functional abnormalities present from intrauterine life, contributing significantly to neonatal morbidity and mortality, especially in low- and middle-income countries. These conditions often require early surgical intervention, yet limited diagnostic and treatment facilities hinder timely care. Common anomalies in pediatric surgery include gastrointestinal malformations, neural tube defects, and abdominal wall defects.
Methods:This hospital-based cross-sectional descriptive study was conducted over one year at the Department of Pediatric Surgery, TMSSMedical College Hospital and Private Camber, Bogura, Bangladesh from January to December 2024. A total of 135 pediatric patients (aged 0–5 years) with structural congenital anomalies requiring surgical evaluation were selected through purposive sampling from (start) to (end). Data were collected via structured interviews with guardians, clinical examinations, antenatal records, and surgical findings. Variables included demographics, obstetric history, anomaly type, surgical interventions, and outcomes. Patients with acquired anomalies or incomplete data were excluded. Data were analyzed using SPSS version 26.0, with results summarized using descriptive statistics and presented in tables.
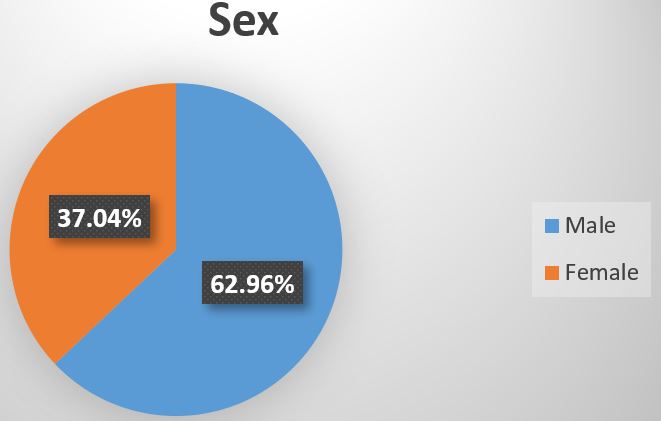
Result:The study revealed that most pediatric patients with congenital anomalies were aged 1–5 years (33.33%) or neonates (29.63%), with a male predominance (62.96%). Normal vaginal delivery was more common (59.26%), and antenatal detection of anomalies was low (18.52%). Anorectal malformation (22.22%) was the most frequent anomaly, followed by cleft lip/palate (14.81%) and neural tube defects (11.11%). Surgical intervention was required in 81.48% of cases, mostly elective. Postoperative complications occurred in 14.81%, and 70.37% had favorable outcomes. However, 11.11% faced complications, another 11.11% were referred, and 3.70% died. The findings highlight the need for improved prenatal diagnosis and early intervention.
Conclusion:The study reveals a high burden of congenital anomalies in Bangladeshi pediatric surgical patients, notably anorectal malformations, cleft lip/palate, and neural tube defects. Most required early surgery. Limited antenatal detection and notable complications highlight the urgent need for improved prenatal screening, early diagnosis, and strengthened pediatric surgical care.
Downloads
References
2. Dolk H, Loane M, Garne E. The prevalence of congenital anomalies in Europe. Rare diseases epidemiology. 2010:349-64.
3. Christianson AL, Howson CP, Modell B. Global report on birth defects: the hidden toll of dying and disabled children. March of Dimes Birth Defects Foundation; 2006.
4. Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bulletin of the World Health Organization. 2008 Jun;86(6):480-7.
5. Ameh EA, Bickler SW, Lakhoo K, Nwomeh BC, Poenaru D, editors. Pediatric Surgery: a comprehensive textbook for Africa. Springer Nature; 2020 Nov 23.
6. Abdou MS, Sherif AA, Wahdan IM, Ashour KS. Pattern and risk factors of congenital anomalies in a pediatric university hospital, Alexandria, Egypt. Journal of the Egyptian Public Health Association. 2019 Dec;94:1-9.
7. Francine R, Pascale S, Aline H. Congenital anomalies: prevalence and risk factors. mortality. 2014;1(2):10-3189.
8. Bhide P, Gund P, Kar A. Prevalence of congenital anomalies in an Indian maternal cohort: healthcare, prevention, and surveillance implications. PloS one. 2016 Nov 10;11(11):e0166408.
9. Botto LD, Lisi A, Bower C, Canfield MA, Dattani N, De Vigan C, De Walle H, Erickson DJ, Halliday J, Irgens LM, Lowry RB. Trends of selected malformations in relation to folic acid recommendations and fortification: an international assessment. Birth Defects Research Part A: Clinical and Molecular Teratology. 2006 Oct;76(10):693-705.
10. Virupakshappa PM, Rajendra N. Burden and spectrum of neonatal surgical diseases in a tertiary hospital: a decade experience. Int J ContempPediatr. 2018 May;5(3):798-803.
11. Magwesela FM, Rabiel H, MlelwaMung'ong'o C. Pattern of congenital anomalies among pediatric surgical patients in a tertiary care hospital in northern Tanzania. World Journal of Pediatric Surgery. 2022 Jul 8;5(4):e000410.
12. Chowdhury TK, Kabir SH, Alam MA, Chowdhury MT, Khan R, Farhad T, Al Farooq MA. Prevalence and pattern of birth defects among pediatric surgical patients: a 12-year analysis in a tertiary-level government hospital in Bangladesh. Asian J Med Health. 2020;4:84-93.
13. Madrid L, Varo R, Sitoe A, Bassat Q. Congenital and perinatally-acquired infections in resource-constrained settings. Expert review of anti-infective therapy. 2016 Sep 1;14(9):845-61.
14. Ahmed W, Dey D, Farid R. Prevalence and pattern of congenital anomalies and its outcome at Chattagram Maa-O-Shishu General Hospital. Chattagram Maa-O-Shishu Hospital Medical College Journal. 2017 Dec 26;16(1):22-5.
15. Tenali AS, Kamalakannan SK, Jayaraman KK. Spectrum of congenital anomalies of neonates in a tertiary care hospital in Southern India. Int J ContempPediatr. 2018 Mar;5(2):314-9.
16. Shawky RM, Sadik DI. Congenital malformations prevalent among Egyptian children and associated risk factors. Egyptian Journal of Medical Human Genetics. 2011;12(1).
17. Anane-Fenin B, Opoku DA, Chauke L. Prevalence, pattern, and outcome of congenital anomalies admitted to a neonatal unit in a low-income country—a ten-year retrospective study. Maternal and Child Health Journal. 2023 May;27(5):837-49.
Copyright (c) 2025 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


