Clinical profile and outcome of septic shock in children admitted to a tertiary care referral hospital
Abstract
Background: There is dearth of studies on detailed clinical profile and outcome of pediatric septic shock in India.
Objective: To describe clinical profile and outcome of septic shock in children.
Methods: This retrospective study was conducted from June 2010 to June 2013 in a tertiary care hospital. Case records of children aged 1month to 18 years with diagnosis of septic shock were analyzed.
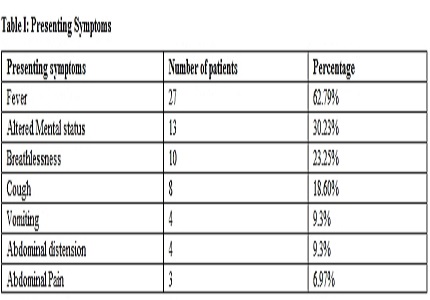
Results: A total of 94(9%) out of 1035 admissions had shock and 53(56.3%) of them had a diagnosis of septic shock. Analysis was done on 43 (M:F, 20:23). The mean age was 3 year (range 1month–14 years). Maximum (48.83%) cases were in infancy. The common presenting symptom was fever (62.79%) followed by altered mental status in 30.23%. Pediatric SIRS criteria was met in 35(81.3%). Most common abnormal lab parameters were elevated liver enzymes (86.04%) followed by anemia (62.79%) and leukocytosis (60.46%). Thrombocytopenia and Coagulopathy was seen in 55.81% and 60.41% respectively. Pneumonia was the commonest etiology (51.1%) followed by cellulitis/abscess in 30.2%. Blood culture was positive in 18.6% and Staphylococcus was the commonest organism. Frequency of MODS was 90.69%. Most (74.41%) cases presented with decompensated shock and 97.67% required inotropes. Majority (88.37%) required mechanical ventilation. The mortality rate was 60.46% and mean duration of PICU was 8.3 days. Anemia, leucopenia, decompensated shock and need for mechanical ventilation were significantly associated with mortality (p<0.05).
Conclusion: Septic shock was the most common type of shock encountered in PICU and carries a high mortality. Maximum numbers of patients were below 1year and pneumonia was the commonest underlying cause.
Downloads
References
2. Watson RS, Carcillo JA. Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med. 2005 May;6(3 Suppl):S3-5. [PubMed]
3. Kutko MC, Calarco MP, Flaherty MB, Helmrich RF, Ushay HM, Pon S, Greenwald BM. Mortality rates in pediatric septic shock with and without multiple organ system failure. Pediatr Crit Care Med. 2003 Jul;4(3):333-7. [PubMed]
4. Dellinger R, Levy M, Rhodes A, Annnae D, Gerlach H, Opal S et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Critical care medicine 2012; 41: 580-637.
5. Militaru M, Martinovici D. Our experience in paediatric sepsis. Jurnalul pediatrului 2005; 8: 26-31.
6. Goldstein B, Giroir B, Adrienne R. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatric. Pediatr Crit Care Med 2005; 6: 2–5.
7. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock. Crit Care Med 2008; 36: 861-3.
8. Singh D, Chopra A, Pooni PA, Bhatia RC. A clinical profile of shock in children in Punjab, India. Indian Pediatr. 2006 Jul;43(7):619-23. [PubMed]
9. Benamer HM, Alsaiti AA, Bofarraj M, Abud H, Tip RM. Diagnosis, management and outcome of sepsis at Benghazi children hospital(1 year review). Pediat Therapeut 5: 267. Doi:10.4172/2161-0665.1000267.
10. Fisher JD, Nelson DG, Beyersdorf H, Satkowiak LJ. Clinical spectrum of shock in the pediatric emergency department. Pediatr Emerg Care. 2010 Sep;26(9):622-5. doi: 10.1097/PEC.0b013e3181ef04b9.
11. Gaines NN, Patel B, Williams EA, Cruz AT. Etiologies of septic shock in a pediatric emergency department population. Pediatr Infect Dis J. 2012 Nov;31(11):1203-5. doi: 10.1097/INF.0b013e3182678ca9.
12. Dahmash NS, Chowdhury NH, Fayed DF. Septic shock in critically ill patients: aetiology, management and outcome. J Infect. 1993 Mar;26(2):159-70. [PubMed]
13. Contran RS, Kumar V, Robbins SL. Shock in fluid and hemodynamic derangements. Robins Pathologic Basis of disease. 114-9.
14. Pollack MM, Fields AI, Ruttimann UE. Sequential cardiopulmonary variables of infants and children in septic shock. Crit Care Med. 1984 Jul;12(7):554-9. [PubMed]
15. Valoor HT, Singhi S, Jayashree M. Low-dose hydrocortisone in pediatric septic shock: an exploratory study in a third world setting. Pediatr Crit Care Med. 2009 Jan;10(1):121-5. doi: 10.1097/PCC.0b013e3181936ab3. [PubMed]
16. Sarthi M, Lodha R, Vivekanandhan S, Arora NK. Adrenal status in children with septic shock using low-dose stimulation test. Pediatr Crit Care Med. 2007 Jan;8(1):23-8. [PubMed]
17. Kaur G, Vinayak N, Mittal K, Kaushik JS, Aamir M. Clinical outcome and predictors of mortality in children with sepsis, severe sepsis, and septic shock from Rohtak, Haryana: A prospective observational study. Indian J Crit Care Med. 2014 Jul;18(7):437-41. doi: 10.4103/0972-5229.136072. [PubMed]
18.Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME, Orr RA. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003 Oct;112(4):793-9.
19. Biban P, Gaffuri M, Spaggiari S, Zaglia F, Serra A, Santuz P. Early recognition and management of septic shock in children. Pediatr Rep. 2012 Jan 2;4(1):e13. doi: 10.4081/pr.2012.e13. Epub 2012 Mar 26. [PubMed]
20. Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999 Dec 4;354(9194):1955-61. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


