Assessment of renal parenchymal changes using isotope renography for genitourinary indications in pediatric age group-a study of 47 cases
Abstract
Background: With the introduction of isotope renography using DMSA (Dimercaptosuccinic acid), more stress than ever has been put on the evaluation of renal parenchyma in a morphologically normal but injured kidney.
Objective: To study the pattern of renal dysfunction and anomalies noted after isotope renography using DMSA.
Materials and methods: A retrospective study was conducted at department of Paediatrics of Amala Institute of Medical Sciences, Thrissur after evaluating the hospital records involving children undergoing isotope renography using DMSA (IRDMSA) for genitourinary indications between August 1st 2012 and August 1st 2013.
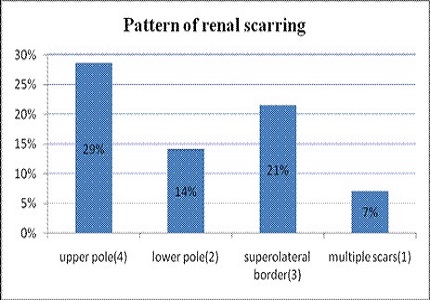
Results: The common indications for IRDMSA were found to be urinary tract infections (UTI) (61.7%), multicystic dysplastic kidneys (MCDK) (12.7%), posterior urethral valve (PUV) (6.3%) and unilateral hydronephrosis (6.3%). Among the UTI group, 10.7% had the evidence of bilateral renal scarring and 42.8% unilateral renal scarring. Only 32.1% had bilaterally normal kidneys. Analysis of 7 cases with significantly reduced differential function (DF< 30/70) showed associated vesicoureteral reflux (VUR) in 100% cases. A male predominance was noticed even though only one case had posterior urethral valve. Right kidney was found to be more susceptible than the left. A study of the scar topography showed majority to be localized to the upper pole and superolateral border. 100% of the MCDKs were found to be non-functional and was not visualized in the renogram.
Conclusion: IRDMSA is a reliable imaging modality in the follow up of acute pyelonephritis in children, detecting structural abnormalities and also for identifying kidneys in children at risk for subsequent renal scarring.
Downloads
References
2. Kawashima A, Sandler CM, Goldman SM. Imaging in acute renal infection. BJU Int. 2000 Jul;86 Suppl 1:70-9. [PubMed]
3. Meyrier A. [Diagnosis of acute pyelonephritis. Contribution of modern imaging]. Presse Med. 1991 Nov 9;20(36):1773-7. [PubMed]
4. Bhatnagar V, Mitra DK, Agarwala S, Kumar R, Patel C, Malhotra AK, Gupta AK. The role of DMSA scans in evaluation of the correlation between urinary tract infection, vesicoureteric reflux, and renal scarring. Pediatr Surg Int. 2002 Mar;18(2-3):128-34.
5. Conway JJ. The role of scintigraphy in urinary tract infection. Semin Nucl Med. 1988 Oct;18(4):308-19. [PubMed]
6. Sixt R, Stokland E. Assessment of infective urinary tract disorders. Q J Nucl Med. 1998 Jun;42(2):119-25. [PubMed]
7. Haycock GB. A practical approach to evaluating urinary tract infection in children. Pediatr Nephrol. 1991 Jul;5(4):401-2; discussion 403. [PubMed]
8. Smellie JM, Rigden SP, Prescod NP. Urinary tract infection: a comparison of four methods of investigation. Arch Dis Child. 1995 Mar;72(3):247-50. [PubMed]
9. Rushton HG, Majd M. Dimercaptosuccinic acid renal scintigraphy for the evaluation of pyelonephritis and scarring: a review of experimental and clinical studies. J Urol. 1992 Nov;148(5 Pt 2):1726-32. [PubMed]
10. Guermazi F, Lenoir P, Verboven M, Smets A, Braeckman J, Jonckheer MH, Piepsz A. [Technetium 99m labeled dimercaptosuccinic acid (99m Tc-DMSA) scintigraphy in the diagnosis and follow-up of urinary infections in children]. Arch Fr Pediatr. 1993 May;50(5):391-8. [PubMed]
11. Rodriguez MM. Congenital Anomalies of the Kidney and the Urinary Tract (CAKUT). Fetal Pediatr Pathol. 2014 Oct-Dec;33(5-6):293-320. doi: 10.3109/15513815.2014.959678. Epub 2014 Oct 14. [PubMed]
12. Goldman M, Lahat E, Strauss S, Reisler G, Livne A, Gordin L, Aladjem M. Imaging after urinary tract infection in male neonates. Pediatrics. 2000 Jun;105(6):1232-5. [PubMed]
13. Lin CH, Yang LY, Wamg HH, Chang JW, Shen MC, Tang RB. Evaluation of imaging studies for vesicoureteral reflux in infants with first urinary tract infection. Acta Paediatr Taiwan. 2007 Mar-Apr;48(2):68-72.
14. Sunilkumar N M, Sasikumar, Gayathrivarma N, KrishnanParvathy V. Xanthogranulomatous Pyelonephritis in a 2 month Old Infant-Case Report. Pediatric Oncall July-September ,Art #49. 2014 July 01;11:( 3) Art #49,DOI: 10.7199/ped.oncall.2014.49.
15. Smokvina A, Grbac-Ivanković S, Girotto N, Dezulović MS, Saina G, Barković MM. The renal parenchyma evaluation: MAG3 vs. DMSA. Coll Antropol. 2005 Dec;29(2):649-54. [PubMed]
16. Gordon I, Evans K, Peters AM, Kelly J, Morales BN, Goldraich N, Yau A. The quantitation of 99Tcm-DMSA in paediatrics. Nucl Med Commun. 1987 Aug;8(8):661-70. [PubMed]
17. Sarhan OM, Alghanbar M, Alsulaihim A, Alharbi B, Alotay A, Nakshabandi Z. Multicystic dysplastic kidney: Impact of imaging modality selection on the initial management and prognosis. J Pediatr Urol. 2014 Aug;10(4):645-9,Epub 2014 Mar 29. [PubMed]
18. Hains D.S, Bates C.M, Ingraham.S, Schwaderer A.L,Management and etiology of the unilateral multicystic dysplastic kidney: a review Pediatr Nephrol. 2009 Feb;24(2):233-41. doi: 10.1007/s00467-008-0828-8. Epub 2008 May 15. [PubMed]
19. Singh JK, Kanojia RP, Narasimhan KL. Multicystic dysplastic kidney in children--a need for conservative and long term approach. Indian J Pediatr. 2009 Aug;76(8):809-12. doi: 10.1007/s12098-009-0117-y. Epub 2009 Apr 16. [PubMed]
20. Krzemień G, Roszkowska-Blaim M, Kostro I, Wojnar J, Karpińska M, Sekowska R. Urological anomalies in children with renal agenesis or multicystic dysplastic kidney. J Appl Genet. 2006;47(2):171-6. [PubMed]
21. de Lucas C, Nocea A, San RJ, Espínola B, Ecija JL, Vázquez Martul M. [Solitary kidney. Study of renal morphology and function in 95 children]. Nefrologia. 2006;26(1):56-63. [PubMed]
22. Sánchez Catalicio J, Gallego Peinado M, Pérez Angel F, Martinez Martínez MT, González Rodríguez JD, Contreras Gutiérrez JF.Megaureter detection through renal scintigraphy scan: Prune-Belly syndrome. . Rev Esp Med Nucl Imagen Mol. 2015 Dec 21. pii: S2253-654X(15)00166-3. doi: 10.1016/j.remn.2015.11.003. [PubMed]
23. Metwalley KA, Farghalley HS, Abd-Elsayed AA. Prune belly syndrome in an Egyptian infant with Down syndrome: a case report. J Med Case Rep. 2008 Oct 2;2:322. doi: 10.1186/1752-1947-2-322.
24. Seidel NE, Arlen AM, Smith EA, Kirsch AJ. Clinical manifestations and management of prune-belly syndrome in a large contemporary pediatric population. Urology. 2015 Jan;85(1):211-5. doi: 10.1016/j.urology.2014.09.029. Epub 2014 Nov 8. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


