To study the effectiveness of indigenous bubble CPAP in management of respiratory distress in newborns
Abstract
Background: CPAP has become a useful in management of respiratory distress, especially in preterms. CPAP delivers a continuous distending pressure via the neonates pharynx to the upper and lower airways. The main indication for use of CPAP is RDS.
Aim of study: To study the effectiveness of indigenous bubble CPAP in management of respiratory distress in newborn and to determine its outcome.
Setting: Department of Pediatrics, MGM Medical College and MY Hospital, Indore during the period February-July 2005.
Design: Prospective Observational Study.
Method: This study was carried out on inborn neonates in the NICU of MY Hospital over a period of six months. Matched controls were taken from admissions during previous four months. It included the newborns developing respiratory distress with grunting and chest retractions within 6 hours of birth whose severity was measured by Silverman Anderson Score and oxygen saturation.Neonates with increasing Silverman Anderson Score or Oxygen saturation falling below 85%were taken on CPAP and their outcome studied.
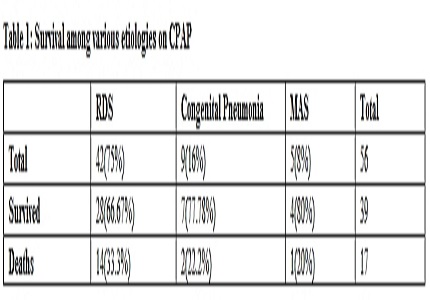
Result: There were 42 RDS cases in the study group of which 28 survived and 14 died. Indigenous BUBBLE CPAP was beneficial in managing babies with RDS.
Conclusion: Indigenous BUBBLE CPAP is an effective and non-invasive way to provide ventilation in a setup with limited resources. It can be used to manage respiratory distress due to RDS, congenital pneumonia & MAS. It resulted in significant reduction in mortality but prognosis was bad in those who required CPAP >8 cm H2O.
Downloads
References
2. Silverman, W. and Anderson, D .: Pediatrics 17:1, 1956. Copyright American Academy of Pediatrics
3. Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK. Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333-40..
4. Singh M, Deorari AK, Paul VK, Mittal M, Shankar S, Munshi U, et al. Three year experience with neonatal ventilation from a tertiary care hospital in Delhi. ndian Pediatr. 1993 Jun;30(6):783-9.
5. Singh M, Deorari AK, Agarwal R, Paul VK. Assisted ventilation for hyaline membrane disease. Indian Pediatr. 1995 Dec;32(12):1267-74.
6. P.P. Maiya, D. Viswanath, S. Hegde, T.P. Srinivas, Shivprasad, C.C. Shantala, P. Umakumaran, Naveen B. And R.K. Hegde, Mechanical ventilation of new borns: experience from a level-II NICU 1275 Indian Pediatrics 1995, 32:1-12.
7. Maiya PP, Vishwanath D, Bhat S, Karthik NN, Shenoi A, Joseph T. Neonatal Ventilation. 15th Annual Convention of the National Neonatology Forum, Patna, 1995.
8. Millar D, Kirpalani H. Benefits of noninvasive ventilation. Indian Pediatr. 2004 Oct;41(10):1008-17.
9. Gittermann et al. 1997. Pediatric and neonatal mechanical ventilation : from basics to clinical practice, page no. 397.
10. Ho JJ, Henderson-Smart DJ, Davis PG. Early versus delayed initiation of continuous distending pressure for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2002; (2): CD002975. Oxford: Update Software Ltd.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


