Comparative study of procalcitonin versus c-reactive protein in the diagnosis of sepsis in children below 16 years-a single centre observational study
Abstract
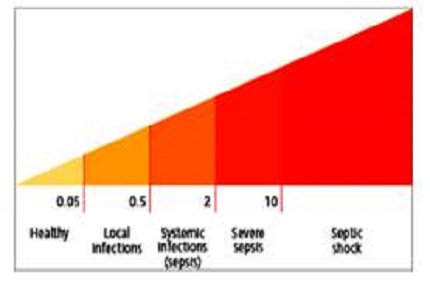
Introduction: Given the limitation of non-specific nature of signs, symptoms and physical examination in diagnosing sepsis; especially in young children, a diagnostic marker that will aid in an early diagnosis is needed. Procalcitonin satisfies most of the criteria for smart biomarker of sepsis. The present study is done to compare procalcitonin (PCT) with C-reactive protein (CRP) as a diagnostic marker of sepsis in children.
Materials & Methods: A prospective observational study was done in the Department of Paediatrics, ASRAM Medical College and Hospital, Eluru from July 2015 to June 2016. Children admitted to PICU during the above tenure are included in the study. Specific inclusion and exclusion criteria are formulated with a sample size of 100. Procalcitonin level is analyzed by enzyme linked immunoluminometric assay using Elecsys Brahms PCT kit.CRP analysis is done using immunoturbidometry which is a quantitative method.
Results: Out of 100 children 72 have sepsis. The mean procalcitonin level in children with sepsis is 19.09 ± 24.53 ng/ml compared to 0.34 ± 0.49 ng/ml in children without sepsis. In comparing sepsis with asepsis, PCT (Cutoff value of 0.58ng/ml) have a better sensitivity (90.3%) and specificity (92.9%) than CRP (Cut off value of 0.7mg/dl) sensitivity of 87.5% and specificity of 57.1%.
Conclusion: PCT offers better sensitivity and specificity than CRP, to differentiate sepsis from asepsis. In febrile children PCT is a better diagnostic marker of sepsis than CRP.
Downloads
References
2. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993 Feb 27;341(8844):515-8. [PubMed]
3. Russwurm S, Wiederhold M, Oberhoffer M, Stonans I, Zipfel PF, Reinhart K. Molecular aspects and natural source of procalcitonin. Clin Chem Lab Med. 1999 Aug;37(8):789-97. [PubMed]
4. Oberhoffer M, Stonans I, Russwurm S, Stotane E, Vogelsang H, Junker U, et al: Procalcitonin expression in human peripheral blood mononuclear cells and it’s modulation by lipopolysaccharides and sepsis –related cytokines in vitro. J Lab Clin Med. 1999;134: 49-55.
5. Jaresová M, Stríz I, Cermáková J, Lácha J, Sedlácek J, Mudra K, Hána I, Vítko S. Serum procalcitonin concentrations in transplant patients with acute rejection and bacterial infections. Immunol Lett. 1999 Sep 1;69(3):355-8.
6. Turner D, Hammerman C, Udensky BR, Schlesinger Y, Goai C, Schimmel MS. Procalcitonin in preterm infants during the first few days of life:introducing an age related nomogram. Arch Dis Child Fetal Neonatal 2006; 91: 283 – 286. [PubMed]
7. Ng PC, Cheng SH, Chui KM, Fok TF, Wong MY, Wong W, Wong RP, Cheung KL. Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 1997 Nov;77(3):F221-7. [PubMed]
8. Paolo Pecile, ElisabettaMiorin, Carla Romanello, EdmondoFalleti, Francesca Valent, Francesco Giacomuzzi, and Alfred Tenore,Procalcitonin: A Marker of Severity of Acute Pyelonephritis among Children.Pediatrics 2004; 114: e249 –e254.
9. Chia-Hung Yo, Pei-Shan Hsieh, Si-Huei Lee, Jiunn-Yih Wu, Shy-Shin Chang, Kuang-ChauTasi, et al. Comparison of the Test Characteristics of Procalcitonin to C-Reactive Protein and Leukocytosis for the Detection of Serious bacterial Infections in Children Presenting With Fever Without Source: A Systematic Review and Meta-analysis. Ann Emerg Med. 2012; 60: 591-600.
10. Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005 Jan;6(1):2-8.
11. David A. Turner and Ira M.Cheifetz.Shock. In: Robert M. Kliegman, Bonita F. Stanton, Joseph W. St. Gemelll, Nina F. Schor, Richard E. Behrman, editors. Nelson textbook of paediatrics.Philadelphia,Elsevier; 2016 20thed p. 517-522.
12. Dominique Gendrel, Josette Raymond, Marcel Assicot, Florence Moulin, Jean-Luc Iniguez, Pierre Lebon, et al. Measurement of Procalcitonin Levels in Children with Bacterial or Viral Meningitis Clinical Infectious Diseases 1997; 24:1240–1242.
13. Corsino Rey, Irene García-Hernández, Andrés Concha, Pablo Martínez-Camblor, Marta Botrán, Alberto Medina, Belén Prieto and Jesús López-Herce Pro-adrenomedullin, pro-endothelin-1, procalcitonin, C-reactive protein and mortality risk in critically ill children: a prospective study Critical Care 2013, 17: R240 : p1-9.
14. Fernández Lopez A, Luaces Cubells C, García García JJ, Fernández Pou J. Procalcitonin in pediatric emergency departments for the early diagnosis of invasive bacterial infections in febrile infants: results of a multicenter study and utility of a rapid qualitative test for this marker. Pediatr Infect Dis J. 2003 Oct; 22(10): 895-903.
15. Andreola B, Bressan S, Callegaro S, Liverani A, Plebani M, Da Dalt L. Procalcitonin and C-reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department. Pediatr Infect Dis J. 2007 Aug; 26(8): 672-677.
16. Carrol ED, Newland P, Riordan FA, et al. Procalcitonin as a diagnostic marker of meningococcal disease in children presenting with fever and a rash. Arch Dis Child 2002; 86: 282–285. [PubMed]
17. Vincenzo Maniaci, Andrew Dauber, Scott Weiss, Eric Nylen, Kenneth L. Becker, Richard Bachur. Procalcitonin in Young Febrile Infants for the Detection of Serious Bacterial Infections. Pediatrics 2008; 122: 701–710.
18. Mark Hatherill, Shane M Tibby, Kim Sykes, Charles Turner, Ian A Murdoch Diagnostic markers of infection: comparison of procalcitonin with C reactive protein and leucocyte count. Arch Dis Child 1999; 81: 417–421.
19. Liliana Simon, France Gauvin, Devendra K. Amre, Patrick Saint-Louis, and Jacques LacroixSerum Procalcitonin and C-Reactive Protein Levels as Markers of Bacterial Infection: A Systematic Review and Meta-analysis Clinical Infectious Diseases 2004; 39: 206–17. [PubMed]
20. Deis JN, Creech CB, Estrada CM, Abramo TJ. Procalcitonin as a marker of severe bacterial infection in children in the emergency department. Pediatr Emerg Care. 2010; 26: 51–60. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


