Incidence of congenital anomalies in neonates – a tertiary care experience
Abstract
Introduction: Congenital malformations represent a defect in the morphogenesis during fetal life. Since the introduction of primary health care, congenital malformations have emerged as one of the commonest causes of perinatal mortality. Hence timely detection and intervention can decrease the morbidity and mortality associated with the congenital anomalies.
Aims and Objectives: To study the incidence of congenital anomalies among live births, term, and preterms, to classify the congenital anomalies and study the underlying risk factors and to study the immediate outcome of congenital malformations in hospital delivered neonates.
Methods: This was a prospective study in which total live births in a duration of 6 months from August 2018 to January 2019 were studied. Data were obtained in the form of total live births-preterm and full term. The congenital anomalies were identified within 24 hours and classified according to the system involved. The information regarding maternal risk factors, age of the mother, family history, previous sibling death, antenatal detection, MRI and CT findings were studied. Detailed history, examinations, and investigations were carried out to identify etiological factors. The further outcome in the form of morbidity, mortality, and intervention was studied.
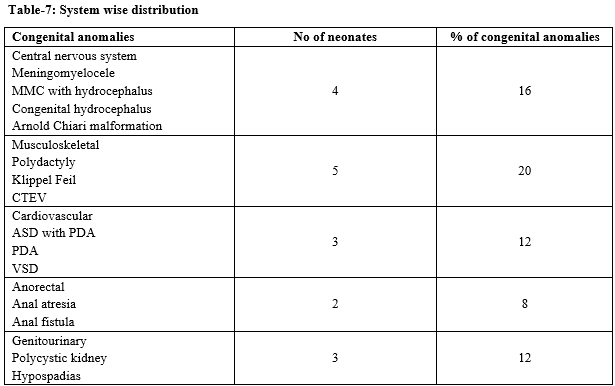
Results: The total incidence of CM among live birth was 6.1%. The incidence among term neonates was 5.1% and among preterms was 33%. The most common system involved was gastrointestinal followed by musculoskeletal, neurological and cardiac (mention percentages).
Conclusions: The overall incidence of congenital anomalies among live birth was 6.1%.The incidence in full-term was and incidence in preterms was 5.1% and 33% respectively. Male gender, multiparity, and consanguinity were identified as risk factors. Gastroesophageal anomalies were the most common followed by musculoskeletal, neurological and cardiac.
Downloads
References
Evaluation of Infant with Single or Multiple Congenital Anomalies. Guidelines American College of Medical Genetics. Available from: http://www.health.ny.gov/nysdoh/dpprd/exec.htm.
Obu HA, Chinawa JM, Uleanya ND, Adimora GN, Obi IE. Congenital malformations among newborns admitted in the neonatal unit of a tertiary hospital in Enugu, South-East Nigeria-a retrospective study. BMC Res Notes. 2012;5:177. doi: http://dx.doi.org/10.1186/1756-0500-5-177.
Kucik JE, Alverson CJ, Gilboa SM, Correa A. Racial/ethnic variations in the prevalence of selected major birth defects, metropolitan Atlanta, 1994-2005. Public Health Rep. 2012;127(1):52-61. doi: https://doi.org/10.1177/003335491212700106.
Park K. Congenital malformations. In: Park K, editor. Park’s Text book of Preventive and Social Medicine. 15th ed. Jabalpur: Banarsidas Bhanot Publishers; 2005. p. 379-380.
Patel KG, Chaudhary C. Study of congenital malformations in newborns: A hospital based prospective study. Int J Contemp Pediatr. 2017;4(4):1409-1413. doi: http://dx.doi.org/10.18203/2349-3291.ijcp20172676.
Padmanabhan R, Venkatasubramanian R, Heber A. Prevalence and Pattern of Congenital Malformations among Neonates in a Medical College Hospital - A Retrospective Study. Int J Sci Stud. 2019;6(12):28-31.
Abdolahi HM, Maher MH, Afsharnia F. Dastgir. Prevalence of Congenital Anomalies: A Community-Based Study in the Northwest of Iran. ISRN Pediatr. 2014. doi: https://doi.org/10.1155/2014/920940
Alijahan R, Mirzarahimi M, Ahmadi-Hadi P, Hazrati S. Prevalence of Congenital Abnormalities and Its Related Risk Factors in Ardabil, Iran. Majallah-i Zanan, Mamai va Nazai-i Iran. 2013;16(54):16-25.
International statistical classification of diseases and related health problems, 10th revision. Geneva: World Health Organization; 2010.
Taksande A, Vilhekar K, Chaturvedi P, Jain M. Congenital malformations at birth in central India: A rural medical college hospital-based data. Indian J Hum Genet 2010;16(3):159-163. doi: http://dx.doi.org/10.4103/0971-6866.73412.
El Koumi MA, Al Banna EA, Lebda I. Pattern of congenital anomalies in newborn: a hospital-based study. Pediatr Rep. 2013;5(1). doi: http://dx.doi.org/10.4081/pr.2013.e5.
Malla BK. One year review study of congenital anatomical malformation at birth in maternity hospital (Prasutigriha), Thapathali, Kathmandu. Kathmandu Univ Med J (KUMJ) 2007;5:557-60.
Dutta HK, Bhattacharyya NC, Sarma JN, Giriraj K. Congenital malformations in Assam. J Indian Assoc Pediatr Surg 2010;15:53-5. doi: http://dx.doi.org/10.4103/0971-9261.70639.
Mohammad K. Gandhi1, Upendra Rameshbhai Chaudhari1, Nilesh Thakor. A study on incidence of congenital anomalies in new borns and their association with fetal factors: a prospective study. Int J Res Med Sci. 2016;4(4):1200-1203. doi: http://dx.doi.org/10.18203/2320-6012.ijrms20160809.
Mohanty C. Congenital anomalies in newborn. A study of 10,874 consecutive birth. J Anatomy Soc India. 1989;38:2.
S. Swain, A. Agrawal B.D. Bhatia. Congenital Malformations At Birth. Indian Pediatr. 1994;31(10):1187-1191.
Sarkar S, Patra C , Dasgupta M, Nayek K, Karmakar P. Prevalence of Congenital Anomalies in Neonates and Associated Risk Factors in a Tertiary Care Hospital in Eastern India. J Clin Neonatol. 2013;2(3):131-134. doi: http://dx.doi.org/10.4103/2249-4847.119998.
Kokate P, Bang R. Study of congenital malformation in tertiary care centre, Mumbai, Maharashtra, India. Int J Reprod Contracept Obstet Gynecol. 2017;6(1):89-93. http://dx.doi.org/10.18203/2320-1770.ijrcog20164638
Suguna Bai NS, Mascarene M, Syamalan K, Nair PM. An etiological study of congenital malformation in the newborn. Indian Pediatr. 1982;19(12):1003-1007.
Desai N, Desai A. Congenital anomalies: A prospective study at TN medical college and BYL Nair hospital Mumbai. Bombay Hosp J. 2006;48:109-114.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


