Evaluation of acid base status and outcome of neonatal respiratory distress
Abstract
Objective: Both pulmonary and extra pulmonary causes could present as tachypnea and respiratory distress. We have planned a study to evaluate acid base status and outcome of neonatal respiratory distress.
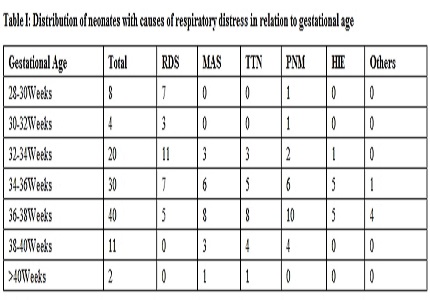
Methods: A prospective study carried on neonates admitted in intensive care unit from 1st November 2014 to 31st October 2015 in Department of Paediatrics of a tertiary care centre of UP. Ethical Clearance was taken by Ethics Committee of the college. Newborns brought to our NICU with respiratory distress were included in study randomly. After detailed clinical history, examination, arterial blood was taken in all the babies for ABG analysis with necessary precautions along with other routine investigation and stabilization of the baby.
Results: A total of 115 neonates with respiratory distress were selected for study, out of these about 24.34% had normal pH, 45.21% had metabolic acidosis, 21.73% neonates had respiratory acidosis and 8.69% had mixed pH disorder. Neonates having respiratory distress with normal pH 85.71% were discharged from the hospital, 7.14% went LAMA and 7.14% expired during the treatment. Neonates having respiratory distress with abnormal pH 77.01% were discharged from the hospital, 2.29% went LAMA and 20.68% expired during the treatment.
Conclusion: The expiry rate was significantly higher in neonates having abnormal pH with respiratory distress than in neonates with normal pH with respiratory distress (p<0.05).
Downloads
References
2. Diwakar KK. Clinical approach to Respiratory Distress in Newborn. Indian J Pediatr (Supplement- optimum pulmonary care of neonates) 2003;70: S53 – S59. [PubMed]
3. Kumar A, Bhatnagar V. Respiratory distress in neonates. Indian J Pediatr. 2005 May;72(5):425-8. [PubMed]
4. Brouillette RT, Waxman DH. Evaluation of the newborn's blood gas status. National Academy of Clinical Biochemistry. Clin Chem. 1997 Jan;43(1):215-21. [PubMed]
5. Quigley R, Baum M. Neonatal acid base balance and disturbances. Semin Perinatol. 2004 Apr;28(2):97-102. [PubMed]
6. Lekhwani S, Shanker V, Gathwala G, Vaswani ND. Acid-base disorders in critically ill neonates. Indian J Crit Care Med. 2010 Apr;14(2):65-9. doi: 10.4103/0972-5229.68217. [PubMed]
7. Seaborn T, Simard M, Provost PR, Piedboeuf B, Tremblay Y. Sex hormone metabolism in lung development and maturation. Trends Endocrinol Metab. 2010 Dec;21(12):729-38. doi: 10.1016/j.tem.2010.09.001. [PubMed]
8. Bresson E, Seaborn T, Côté M, Cormier G, Provost PR, Piedboeuf B, Tremblay Y. Gene expression profile of androgen modulated genes in the murine fetal developing lung. Reprod Biol Endocrinol. 2010 Jan 8;8:2. doi: 10.1186/1477-7827-8-2. [PubMed]
9. Santosh S, Kushal Kumar K, Adarsha E. A clinical study of respiratory distress in newborn and its outcome. Indian Journal of Neonatal Medicine and Research 2013; 2(1):2-4.
10. Jing Liu. Respiratory Distress Syndrome in Term Neonates: Published online 2014 Mar 1. doi: 10.5152/balkanmedj.2014.8733.
11. Anitha B. Sethi et al., IOSR Journal of Dental and Medical Sciences 2015;14(12): 35-38.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


