Influence of high-risk factors on early neurodevelopmental outcome of high-risk newborns and role of follow up compliance
Abstract
Aims and Objective: Influence of high-risk factors on early Neurodevelopmental and Neuromotor outcome at 3 months of corrected age and role of continued Newborn follow up care.
Participants: All high-risk newborn discharged from tertiary care level NICU were enrolled for study at discharge.
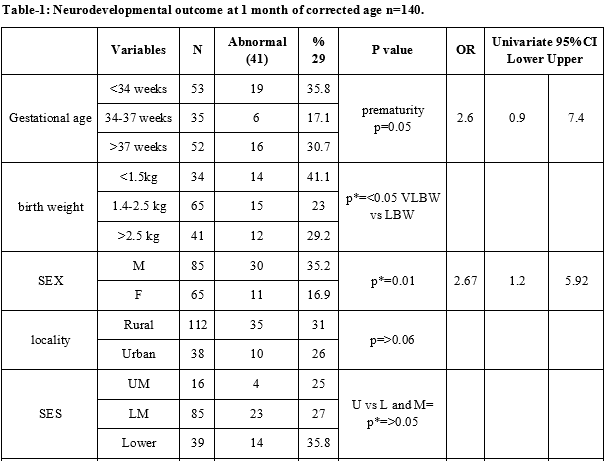
Method: In this prospective observational study, the influences of various sociodemographic factors as prematurity, birth weight, maternal education, family size, clinical profile, sociodemographic factors, parity, feeding patterns and follow up compliance on the neurodevelopmental outcome at 1 and 3 months of corrected age were studied.
Results: Prematurity, ELBW and VLBW infants, Male infants, Low socioeconomic status, disease-causing CNS injury ( Severe Birth asphyxia, meningitis), poor maternal education, mixed and top feeding, longer duration of NICU stay, poor follow-up attendance and compliance were significantly( p=<0.05) associated with poor neurodevelopmental outcome at 1 and 3 month of corrected age.
Conclusion: Collaborative efforts shall be made to educate the parents of high-risk newborns towards the need and importance of neonatal follow-up and early stimulation and intervention therapy to decrease the future neurodevelopment abnormality. Special attention shall be given to premature LBW infants of the less-educated mother, of poor socioeconomic status and residing in distant rural areas having poor access to specialized center-based services.
Downloads
References
National Family Health Survey (NFHS-4) NFHS-4 fact sheets for key indicators based on final data. Available at http://rchiips.org/NFHS/factsheet_NFHS-4.shtml.
Xiong T, Gonzalez F, Mu DZ. An overview of risk factors for poor neurodevelopmental outcomes associated with prematurity. World J Pediatr. 2012;8(4):293-300. doi: https://doi.org/10.1007/s12519-012-0372-2.
Basaran A1, Karadavut KI. The effect of having a children with cerebral palsy on quality of life, burn-out, depression and anxiety scores: a comparative study. Eur J Phys Rehabil Med. 2013;49(6):815-822. Epub 2013 Nov 28.
Park EY1, Nam SJ., Time burden of caring and depression among parents of individuals with cerebral palsy. Disabil Rehabil. 2019:41(13):1508-1513. doi: https://doi.org/10.1080/09638288.2018.1432705.
Evidence Based Clinical Practice Guidelines. National Neonatology Forum India.
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database of Systematic Reviews. 2015; (11): CD005495. doi: https://doi.org/10.1002/14651858.CD005495.
Brazelton TB, Parker WB, Zuckerman B. Importance of behavioral assessment of the neonate Curr Probl Pediatr. 1976;7(2):1-82. doi: https://doi.org/10.1016/s0045-9380(76)80013-8.
Meisels SJ, Tison A. Can developmental screening tests identify children who are developmentally at risk? C: Neurological evaluateion of maturity of newborn, Arch. Dis Pediatrics. 1989;83(4):578-585.
Amile Tison, C: Neurological evaluateion of maturity of newborn, Arch Dis. 1968;43(227):89-93. doi: https://dx.doi.org/10.1136%2Fadc.43.227.89.
Salmaso N, Tomasi S Vaccarino FM. Neurogenesis and maturation in neonatal brain injury. Clin Perinatol. 2014;41(1):22939. doi: https://doi.org/10.1016/j.clp.2013.10.007.
Hadfield K, Fearghal O’Brien F, Gerow A. Is level of prematurity a risk/plasticity factor at three years of age? Infant Behav Dev. 2017; 47: 27–39. doi: https://dx.doi.org/10.1016%2Fj.infbeh.2017.03.003.
Spittle AJ, McGinley., Motor trajectories from birth to 5 years of children born at less than 30 weeks’ gestation: early predictors and functional implications. Protocol for a prospective cohort study., JL Physiother. 2016;62(4):2223. doi: https://doi.org/10.1016/j.jphys.2016.07.002.
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database of Systematic Reviews 2015;11:CD005495. doi: https://doi.org/10.1002/14651858.CD005495.
Kolb B, Gibb R. Searching for the principles of brain plasticity and behavior. Cortex. 2014;58:251-260. doi: https://doi.org/10.1016/j.cortex.2013.11.012.
Spinillo A, Montanari L, Infant sex, obstetric risk factors, and 2year neurodevelopmental outcome among preterm infants. Develop Med Child Neurol. 2009;51(7):518–525. doi: https://doi.org/10.1111/j.14698749.2009.03273.
DiPietro JA, Voegtline K M. The gestational foundation of sex differences in development and vulnerability. Neurosci. 2017;342:4-20. doi: https://doi.org/1016/j.neuroscience.2015.07.068.
Thordstein M, Löfgren N, Sex differences in electrocortical activity in human neonates. Neuro Report. 2006;17(11):1165-1168. doi: https://doi.org/10.1097/01.wnr.0000227978.98389.43.
Schoetzau A, Gehring U, Gini Study Group Maternal compliance with nutritional recommendations in an allergy preventive programme. Arch Dis Child. 2002;86(3):180-184. doi: https://doi.org/10.1136/adc.86.3.180.
Prajapati J, Singh J, Bijesh S, Singh HP. Appointment Compliance Among High Risk Newborns. Ind J Pediatr. 2014;81(12):1407-1408. doi: https://doi.org/10.1007/s12098-014-1384-9.
Lechner BE, Vohr BR. Neurodevelopmental Outcomes of Preterm Infants Fed Human Milk: A Systematic Review Clin Perinatol. 2017;44(1):69-83. doi: https://doi.org/10.1016/j.clp. 2016.11.004.
Doyle LW, Anderson PJ, Battin M, Bowen JR, Brown N, Callanan C et al. Long term follow up of high-risk children: who, why and how? BMC Pediatr. 2014;14(1):279. doi: https://doi.org/10.1186/1471243114279.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


