Study of glycemic status, thyroid function and vitamin D3 level in children with β thalassemia major in a tertiary care center
Abstract
Introduction: β thalassemia has emerged as a huge public health problem worldwide. Thyroxine reserve is reduced in multitransfused thalassemia patientsanddiabetes can also be a considerable complication.Vitamin D3 deficiency is noted in thalassemia patients and is related to bone diseases.
Aims and Objectives: Study of glycemicstatus, thyroid function, and vitamin D3 level in children with βthalassemia major.
Method:Socio-demographic information wascollected by using the pretested and predesigned structured pro forma by interview technique. HbA1c level, vitamin D3 level,and thyroid function had been obtained from the lab.
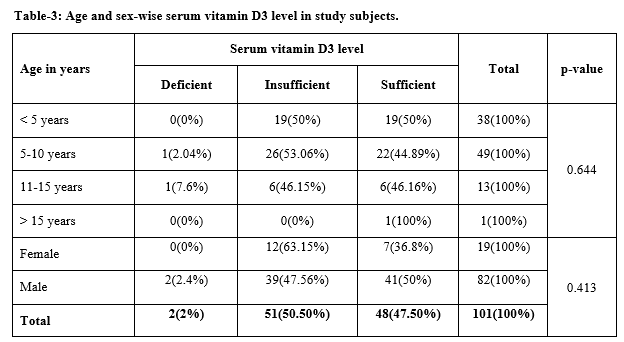
Result:In 89% of subjects TSH levels were normal with a mean value of 5.04.In 10.9%it was increased witha mean value of TSH being 6.67.VitaminD3 level in 2% children was below 20ng/ml, 50.50% had between 21 to 29ng/ml and 47.52% had between 30-60 ng/ml. Vitamin D3 deficiency increased with a higher blood transfusion rate (p-value 0.000). In 88.12%of the study, subjectsHbA1c was normal, 11.18%were inthe pre-diabetic range,and none of the subjects were diabetic as per HbA1C results. The mean value of HbA1C in normal children was 4.79%whereas in prediabetic children mean value of HbA1C was 6.13%.
Conclusion: In the present study multiple endocrine abnormalities were common in multi transfused thalassemia major patients. Prevalence of subclinical hypothyroidism and prediabetes increased with a higher blood transfusion rate and higher serum ferritin level. Prevalence of subclinical hypothyroidism and prediabetes increased with age (p-value <0.05).
Downloads
References
Old J, Harteveld CL, Traeger-Synodinos J, Petrou M, Angastiniotis M, Galanello R. Haematological Methods. InPrevention of Thalassaemias and Other Haemoglobin Disorders: Volume 2: Laboratory Protocols [Internet]. 2nd edition 2012. Thalassaemia International Federation.
Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: An increasing global health problem. Bull World Health Organ. 2001;79(8):704-712.
De VS, Roos M, Gasser T, Fortini M, Raiola G, Galati MC. Impact of long-term iron chelation therapy on growth and endocrine functions in thalassaemia. J Pediatr Endocrinol Metab. 2006;19(4):471-480.
S T, SN R. Thalassemia prevalence in the state of Chhattisgarh: A short-review of the Literature. J Blood Disord Med. 2018;3:5-7.
Malik SA, Syed S, Ahmed N. Frequency of hypothyroidism in patients of b-thalassemia. J Pak Med Assoc. 2010;60(1):17-20.
Eshragi P, Tamaddoni A, Zarifi K, Mohammadhasani A, Aminzadeh M. Thyroid function in major thalassemia patients: Is it related to height and chelation therapy? Casp J Intern Med. 2011;2(1):189-193.
Hashemizadeh H, Noori R. Assessment of Hypothyroidism in Children with Beta-Thalassemia Major in North Eastern Iran. Iran J Pediatic Hematol Oncol. 2012;2(3):123-127.
Rindang C, Batubara JRL, Amalia P, Satari H. Some aspects of thyroid dysfunction in thalassemia major patients with severe iron overload. Paediatr Indones. 2011;51(2):66-72.doi: https://doi.org/10.14238/pi51.2.2011.66-72.
Tsilingiris D, Makrilakis K, Voskaridou E, Pagkrati S, Dalamaga M, Liatis S. Effect of heterozygous beta thalassemia on HbA1c levels in individuals without diabetes mellitus: A cross sectional study. Clin Chim Acta. 2019;494:132-137.doi: https://doi.org/10.1016/j.cca.2019.03.1611.
Metwalley K, El-Saied AR. Glucose homeostasis in Egyptian children and adolescents with β-Thalassemia major: Relationship to oxidative stress. Indian J Endocrinol Metab. 2014;18(3):333-339.doi: https://doi.org/10.4103/2230-8210.131169.
El-Samahy MH, Tantawy AA, Adly AA, Abdelmaksoud AA, Ismail EA, Salah NY. Evaluation of continuous glucose monitoring system for detection of alterations in glucose homeostasis in pediatric patients with β-thalassemia major. Pediatr Diabetes. 2019;20(1):65-72.doi: https://doi.org/10.1111/pedi.12793.
He LN, Chen W, Yang Y,Xie YJ, Xiong ZY, Chen DY, et al. Elevated Prevalence of Abnormal Glucose Metabolism and Other Endocrine Disorders in Patients with β -Thalassemia Major: A Meta-Analysis. Biomed Res Int. 2019. doi: https://doi.org/10.1155/2019/6573497.
El-Hazmi MA, Al-Swailem A, Al-Fawaz I, Warsey AS, Al-Swailem A, et al. Diabetes mellitus in children suffering from β-thalassaemia. J Trop Pediatr. 1994;40(5):261-266.doi: https://doi.org/10.1093/tropej/40.5.261.
Mashhadi MA, Sepehri Z, Heidari Z, Kaykhaei MA, Sargazi A, Kohan F, et al. A cross-sectional study of glycemic status and zinc level in patients with Beta-Thalassemia major. Int J Hematol Stem Cell Res. 2017;11(4):273-280.
Fahim FM, Saad K, Askar EA, Eldin EN, Thabet AF. Growth parameters and vitamin D status in children with thalassemia major in upper Egypt. Int J Hematol Stem Cell Res. 2013;7(4):10-14.
Ahmed Z, . P, Kausar MS, Sinah D. Study of serum calcium, phosphorus and vitamin D status in multitransfused β-thalassemia major children and adolescents of Jharkhand, India. Int J Contemp Pediatr. 2019;6(2):598.doi: http://dx.doi.org/10.18203/2349-3291.ijcp20190694.
Gombar S, Parihar K, Choudhary M. Comparative study of serum ferritin and vitamin D in thalassemia patients with healthy controls. Int J Res Med Sci. 2018;6(2):693.doi: http://dx.doi.org/10.18203/2320-6012.ijrms20180322.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


