Clinical outcome of dysglycaemia in children admitted to pediatric ward at a tertiary care hospital - a prospective study
Abstract
Background: Dysglycaemia (hyper- or hypoglycaemia) in critically ill children has been associated with poor outcome.
Objective: comparison of clinical outcomes in children admitted to Emergency unit of MGM Hospital, Warrangal for acute medical conditions and presenting with euglycaemia or dysglycaemia.
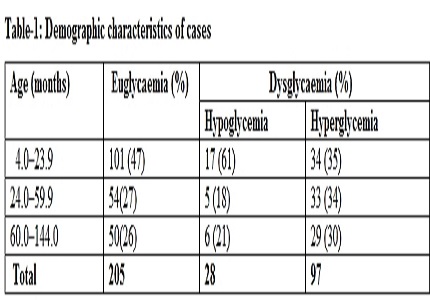
Methods: Five hundred and twenty five subjects aged between 4 months and 12 years were screened out of whom 330 (205 with euglycaemia and 125 with dysglycaemia) were enrolled.
Results: In the dysglycaemia group, 28 (13%) subjects had hypoglycemia and 97 (87%) had hyperglycemia. Overall, there were 101 complications in 125 subjects. The number of subjects with complications was significantly higher in dysglycaemia group (46%) compared to euglycaemia group (8%). Fifty subjects died out of whom 30 had dysglycaemia. Subjects with dysglycaemia were 3 times (95% CI: 1.5–6.0) more likely to die and 4.8 times (95% CI: 3.1–7.5) more likely to develop complications.
Conclusion: Dysglycaemia is associated with increased morbidity and mortality in children with acute medical conditions.
Downloads
References
2. Bhisitkul DM, Morrow AL, Vinik AI, Shults J, Layland JC, Rohn R. Prevalence of stress hyperglycemia among patients attending a pediatric emergency department. Journal of Pediatrics 1994; 124( 4): 547–551.
3. Elusiyan JB, Adejuyigbe EA, Adeodu OO. Hypoglycaemia in a Nigerian paediatric emergency ward. J Trop Pediatr. 2006 Apr;52(2):96-102. Epub 2005 Sep 16.
4. Osier FH, Berkley JA, Ross A, Sanderson F, Mohammed S, Newton CR. Abnormal blood glucose concentrations on admission to a rural Kenyan district hospital: prevalence and outcome. Arch Dis Child. 2003 Jul;88(7):621-5.
5. Kwiatkowski D, Hill AV, Sambou I, Twumasi P, Castracane J, Manogue KR, Cerami A, Brewster DR, Greenwood BM.TNF concentration in fatal cerebral, non-fatal cerebral, and uncomplicated Plasmodium falciparum malaria Lancet. 1990 Nov 17;336(8725):1201-4.
6. Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM.Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics. 2006 Jul;118(1):173-9.
7. Langdon DR, Stanley CA, Sperling MA. Hypoglycemia in the infant and child. In: Sperling MA, editor. Pediatric endocrinology. 3rd edition. Philadelphia: Saunders Elsevier; 2008. pp. 422-423.
8. Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009 May 23;373(9677):1798-807. doi: 10.1016/S0140-6736(09)60553-5. [PubMed]
9. Gupta P, Natarajan G, Agarwal KN. Transient hyperglycemia in acute childhood illnesses: to attend or ignore? Indian J Pediatr. 1997 Mar-Apr;64(2):205-10. [PubMed]
10. Solomon T, Felix JM, Samuel M, Dengo GA, Saldanha RA, Schapira A, Phillips RE. Hypoglycaemia in paediatric admissions in Mozambique. Lancet. 1994 Jan 15;343(8890):149-50. [PubMed]
11. English M, Sauerwein R, Waruiru C, Mosobo M, Obiero J, Lowe B, Marsh K. Acidosis in severe childhood malaria. QJM. 1997 Apr;90(4):263-70. [PubMed]
12. Thien HV, Kager PA, Sauerwein HP. Hypoglycemia in falciparum malaria: is fasting an unrecognized and insufficiently emphasized risk factor? Trends Parasitol. 2006 Sep;22(9):410-5. Epub 2006 Jul 12. [PubMed]
13. Zijlmans W, van Kempen A, Ackermans M, de Metz J, Kager P, Sauerwein H. Glucose kinetics during fasting in young children with severe and non-severe malaria in suriname. Am J Trop Med Hyg. 2008 ;79(4):605-12. [PubMed]
14. Waller D, Krishna S, Crawley J, Miller K, Nosten F, Chapman D, ter Kuile FO, Craddock C, Berry C, Holloway PA, et al. Clinical features and outcome of severe malaria in Gambian children. Clin Infect Dis. 1995 Sep;21(3):577-87. [PubMed]
15. Bjerre JV. [Stress hyperglycemia in a child with severe acute gastroenteritis]. Ugeskr Laeger. 2002 Nov 18;164(47):5524-5. [PubMed]
16. de Groof F , Joosten KF, Janssen JA, de Kleijn ED, Hazelzet JA, Hop WC, Uitterlinden P, van Doorn J, Hokken-Koelega AC. Acute stress response in children with meningococcal sepsis: important differences in the growth hormone/insulin-like growth factor I axis between nonsurvivors and survivors. J Clin Endocrinol Metab. 2002 ;87(7):3118-24.
17. van Waardenburg DA, Jansen TC, Vos GD, Buurman WA .Hyperglycemia in children with meningococcal sepsis and septic shock: the relation between plasma levels of insulin and inflammatory mediators. J Clin Endocrinol Metab. 2006 ;91(10):3916-21. [PubMed]
18. Don M, Valerio G, Korppi M, Canciani M. Hyper- and hypoglycemia in children with community-acquired pneumonia. J Pediatr Endocrinol Metab. 2008 Jul;21(7):657-64. [PubMed]
19. Eltahir EM, El Ghazali G, A-Elgadir TM, A-Elbasit IE, Elbashir MI, Giha HA. Raised plasma insulin level and homeostasis model assessment (HOMA) score in cerebral malaria: evidence for insulin resistance and marker of virulence. Acta Biochim Pol. 2010;57(4):513-20. Epub 2010 Dec 6. [PubMed]
20. Manning L, Laman M, Davis WA, Davis TM. Clinical features and outcome in children with severe Plasmodium falciparum malaria: a meta-analysis. PLoS One. 2014 Feb 6;9(2):e86737. doi: 10.1371/journal.pone.0086737. eCollection 2014. [PubMed]
21. Abdallah TM, Elmardi KA, Elhassan AH, Omer MB, Elhag MS, Desogi MA, Siddig MF, Adam I. Comparison of artesunate and quinine in the treatment of severe Plasmodium falciparum malaria at Kassala hospital, Sudan. J Infect Dev Ctries. 2014 May 14;8(5):611-5. doi: 10.3855/jidc.3813.
22. Kawo NG, Msengi AE, Swai AB, Orskov H, Alberti KG, McLarty DG. The metabolic effects of quinine in children with severe and complicated Plasmodium falciparum malaria in Dar es Salaam. Trans R Soc Trop Med Hyg. 1991;85(6):711-3. [PubMed]
23. Willcox ML, Forster M, Dicko MI, Graz B, Mayon-White R, Barennes H. Blood glucose and prognosis in children with presumed severe malaria: is there a threshold for 'hypoglycaemia'? Trop Med Int Health. 2010 Feb;15(2):232-40. doi: 10.1111/j.1365-3156.2009.02444.x. Epub 2009 Dec 4. [PubMed]
24. Sambany E, Pussard E, Rajaonarivo C, Raobijaona H, Barennes H. Childhood dysglycemia: prevalence and outcome in a referral hospital. PLoS One. 2013 May 31;8(5):e65193. doi: 10.1371/journal.pone.0065193. Print 2013. [PubMed]
25. Achoki R, Opiyo N, English M. Mini-review: Management of hypoglycaemia in children aged 0-59 months. J Trop Pediatr. 2010 Aug;56(4):227-34. doi: 10.1093/tropej/fmp109. Epub 2009 Nov 23. [PubMed]
Copyright (c) 2017 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


